- Genetics are 40%-60% of the Risk
- Personality Traits
- Concurrent Mental Health Disorders
- Developmental Factors
- Social Factors (Getting Along with Others)
- Drug characteristics: All drugs are not created equal
Genetics are 40%-60% of the Risk
Genetic factors play a significant role in SUD. Studies involving twins and people who have been adopted indicate that 40-60% of the risk of developing SUD comes from a genetic vulnerability and many scientists are actively searching for the particular genes involved.
All addictive drugs act on the brain by activating certain reward pathways. These pathways are necessary to reward behaviours that contribute to our survival. For example, we experience pleasure when we eat certain foods, such as fat, salt and sugar, which, from an evolutionary point of view, were important for survival. Drugs bypass the behaviour stage and stimulate the reward pathways directly, usually via dopaminergic neurons. The drugs mimic natural brain peptides, such as endorphins (opioids) and anandamide (cannabis).
For some of us, the reward pathways in our brain are more easily hijacked by drugs. This susceptibility is partially conferred by genes that make our receptors more sensitive to drugs. There are many genes involved and they may or may not be passed on through the generations. It is a very complex field.
The inherited differences involved in drug use and dependence vary for each drug:
- for tobacco, differences in the genes involved in the metabolism of nicotine;
- for alcohol, differences in the genes involved in the metabolism of alcohol and inherited differences in certain brain cell receptors (for serotonin, dopamine and GABA); and
- for opioids, inherited differences in the brain cell receptors for opioids and in the enzymes that metabolize opioids.
Genetic differences may influence many aspects of a person’s drug use. For instance, they may influence how pleasurable a drug is, to what extent it harms health (overdose or long-term effects), how strong the withdrawal symptoms and cravings are, and how easily the person develops tolerance. For example, studies have found that sons of alcoholic fathers respond differently to alcohol than sons of non-alcoholic fathers; they tend to enjoy it more, and they have greater innate tolerance, in other words they can drink greater amounts.
Personality Traits
A new program for schools, Preventure, developed by University of Montreal psychiatry professor Patricia Conrod identifies four main personality traits that put children at risk for addiction:
- Sensation-seeking
- Impulsiveness
- Anxiety sensitivity
- Hopelessness
All of these traits are linked to mental health disorders with the exception of sensation-seeking. The program aims to determine which students have which traits and gives them coping strategies to manage these traits.
Concurrent Mental Health Disorders
SUD can develop from many of the same personality traits that lead to mental health disorders. For example, impulsivity as a personality trait is associated with SUD, Attention Deficit and Hyperactivity Disorder (ADHD) and antisocial personality disorder (ASPD).
Many mental health disorders are associated with an increased risk of SUD, and vice-versa.
Nine percent of the American population meet the criteria for having a personality disorder (PD). Each PD has different traits and criteria, but when these personality traits are inflexible and maladaptive and cause significant functional impairment or subjective distress, they constitute a PD. People with Borderline Personality Disorder (BPD) show a pervasive pattern of instability of interpersonal relationships, self-image, emotions and marked impulsivity. ASPD is characterized by an egocentric identity and self-direction (me first always) and a lack of empathy or capacity for intimacy with others.
Persons with SUD are at increased risk of having a PD. For example, 27% of patients with alcohol use disorder also have a PD, the most prevalent being ASPD and BPD. Also, 54% of patients with other SUDs (except for nicotine) also have a PD, again most commonly ASPD and BPD.
People with ASPD have a 15.5% SUD rate. Bipolar disorder is next at 14.5%. For anxiety disorders it is 4.3%. Post-traumatic stress disorder (PTSD) and ADHD are both associated with SUD. Any serious mental illness, such as schizophrenia or any other psychotic illness increases the chances of developing SUD. For some other mental health disorders the rate of SUD is 40-50% (versus 4-5% for the general population).
Mental health disorders such as anxiety, depression, ADHD or PTSD can lead to problematic substance use as the person tries to treat the symptoms of the mental condition (called “self-medication”). One or two drinks may be effective short term relief for occasional anxiety. However, to someone with PTSD who has a high level of anxiety at all times and is hypervigilant around others it may feel like they need alcohol just to get through each day.
People who are at risk for mental health disorders increase that risk when they chronically misuse drugs. While it is clear that there is a correlation between mental health disorders and problematic substance use, causation has not yet been established in most cases.
There is a fair amount known about the relationship between alcohol use and depression.
- Patients with alcohol use disorder are also at high risk for mood disorders.
- Heavy alcohol use can cause an organic mood syndrome that is clinically indistinguishable from a primary mood disorder. Conversely, patients with a mood disorder are more likely to drink heavily to cope with their low mood – but alcohol can markedly worsen their mood even though it temporarily relieves symptoms. Alcohol is also an independent risk factor for suicide.
- A trial of abstinence will help distinguish primary from alcohol induced mood disorders; the latter will improve markedly after 1-3 months of abstinence, whereas the former won’t.
In fact, all the major drugs (alcohol, opioids, cannabis, benzodiazepines, cocaine and other stimulants) can worsen mood.
A few drugs can cause mental health disorders after years of problematic substance use. Drugs such as ecstasy alter chemicals in the brain that control mood and other behaviors. These alterations can lead to depression or anxiety which can lead to self-medication with other drugs.
Heavy drug use in the adolescent years can lead to mental health disorders such as depression and anxiety later in life. Problematic substance use can impair the cognitive and social development or maturation of the adolescent brain.
Developmental Factors
Early Use
The large majority of patients with SUD report that their problems with alcohol and other drugs began in adolescence. It is therefore not surprising that the earlier a teen experiments with drugs or alcohol, the more likely they will develop problematic use. When SUDs occur in adolescence, they affect key developmental and social transitions, and they can interfere with normal brain maturation. These potentially lifelong consequences make addressing adolescent drug use an urgent matter. Impaired memory or thinking ability and other problems caused by drug use can delay and/or hinder a young person’s social and educational development.
Family
Recent studies have demonstrated the significant, enduring, and protective influence of positive parenting practices on adolescent development. In particular, parental monitoring, open parent-child communication, supervision, and high quality of the parent-child relationship deter involvement in high-risk behavior. The authoritative (as opposed to authoritarian or permissive) parenting style generally leads to the best outcomes for teens. Several studies of parent–child communication and adolescent substance use have indicated that the more parents talk with their children about substance use, the less likely children are to use substances.
Many studies have shown that parental use and abuse of alcohol, tobacco, and other drugs are associated with an increased risk for use by in offspring.
An adolescent’s substance use is related to the substance use of his siblings. Older siblings’ drug use during adolescence and early adulthood has been found to predict future use by a younger sibling. However, the strength of influence by an older sibling is moderated by the quality of the sibling relationship, such that a warm and supportive relationship with an older sibling who uses substances represents a high risk for substance use by the younger sibling. Additionally, the tendency of the younger sibling to follow the older sibling in to substance use occurs more often when the two are the same gender and close in age.
Family disharmony (i.e. high levels of conflict among family members), family disorganization (i.e. lack of stable routines) and low family cohesion/connectedness (i.e. lack of bonds or involvement among family members) are related to increased risk for adolescent substance use.
Trauma
Numerous studies have shown that traumatic childhood experiences make you more susceptible to drug misuse. The greater the stress of your childhood experiences, and the greater the variability in the types of your stress, the greater your risk of developing addiction. The Adverse Childhood Experiences (ACE) study found multiple relationships between severe childhood stress and all types of addictions, including overeating. ACE included abuse (emotional, physical and sexual), neglect, having a parent who struggles with SUD and/or mental health disorders, losing a parent to death or divorce, living in a house with domestic violence and having an incarcerated parent.
Compared to a child with no ACE, one with six or more ACEs is nearly three times more likely to be a smoker as an adult. A child with four or more is five times more likely to become an alcoholic and 60% more likely to become obese. And a male with six ACEs is a staggering 46 times more likely to become an IV drug user later in life than one who has had no severe ACEs.
Aside from childhood trauma, trauma experienced later in life can cause post-traumatic stress disorder and this can be a risk factor for SUD and other mental health disorders. Emergency services personnel and soldiers can be traumatized by their work experiences. Sexual and physical assault can also put people at greater risk for SUD.
Peers
There is no single answer to the question of why young people use substances, but it is clear that peers are a key ingredient. Peer relations, risk taking and substance use intensify during adolescence. Peers take center stage, providing consensual validation for the unique experiences of early adolescence, a safe haven from the adult-run worlds of families and schools, a sounding board for identity quests, a launching pad for romantic relations, and fuel and direction for sensation-seeking and risk-taking behaviors. Alcohol, tobacco, and illicit drug use are typically initiated during adolescence, with rates climbing quickly across middle and high school and into the transition to adulthood, and peers provide the opportunity and social context for substance use initiation and escalation. In particular, the level of marijuana use by an adolescent’s friends is the most reliable predictor of marijuana use.
Spirituality
Several studies have shown that high levels of general religiosity (concern with religious and spiritual issues, seeking strength and guidance from God) reduce risk for substance use and problematic substance use among both adolescents and adults.
Social Factors (Getting Along with Others)
Some researchers believe that drug use and anti-social behaviors are learned predominantly through three sources; the family, the school and peers. Anti-social personality disorder (ASPD), conduct disorder and oppositional-defiant disorder (ODD) go hand-in-hand with addiction. All of these disorders can decrease confidence and the ability to assess social cues. Consequently, children and teens who struggle with these disorders (and their effects on the ways they relate to others) tend to start drug use earlier and use more aggressively and are more than twice as likely as their peers to develop SUD.
Social isolation is also a major risk factor for adolescent SUD. The brain of a socially isolated teen measures risk and reward differently than the brain of a social teen, making isolated teens more sensitive to the rewards of drugs. The research shows that socialization and drugs work on the same pathways within the brain – drugs are literally a way to attempt to get the neurobiological feeling of social connection. Johann Hari, the author of Chasing The Scream, believes that the opposite of addiction is not sobriety. It is connection. He explains this in a You Tube video.
Not all socialization is good. Social insults in early life increase later drug taking. So be careful if trying to encourage an isolated teen into socialization – healthy socialization may be one of the most protective factors against teen drug use, but negative socialization (i.e. being bullied or socializing with a drug-using peer) is a major risk factor.
Drug characteristics: All drugs are not created equal
The dependence potential of a drug varies from substance to substance, and from individual to individual. Dose (potency), frequency of use, pharmacokinetics (the characteristic interactions of a drug and the body in terms of its absorption, distribution, metabolism, and excretion), route of administration (swallowing, snorting, smoking or injecting) and duration of use are critical factors for developing drug dependence.
A Lancet article compared the harm and physical and psychological dependence of 20 drugs, using a scale from zero to three for physical dependence, psychological dependence, and pleasure to create a mean score for dependence. Selected results can be seen in the chart below.
| Drug | Mean | Pleasure | Psychological dependence | Physical dependence |
|---|---|---|---|---|
| Heroin | 3.00 | 3.0 | 3.0 | 3.0 |
| Cocaine | 2.39 | 3.0 | 2.8 | 1.3 |
| Tobacco | 2.21 | 2.3 | 2.6 | 1.8 |
| Barbiturates | 2.01 | 2.0 | 2.2 | 1.8 |
| Alcohol | 1.93 | 2.3 | 1.9 | 1.6 |
| Benzodiazepines | 1.83 | 1.7 | 2.1 | 1.8 |
| Amphetamine | 1.67 | 2.0 | 1.9 | 1.1 |
| Cannabis | 1.51 | 1.9 | 1.7 | 0.8 |
| Ecstasy | 1.13 | 1.5 | 1.2 | 0.7 |
Here is the comprehensive diagram illustrating the results for all 20 substances in terms of harm to users and harm to others.
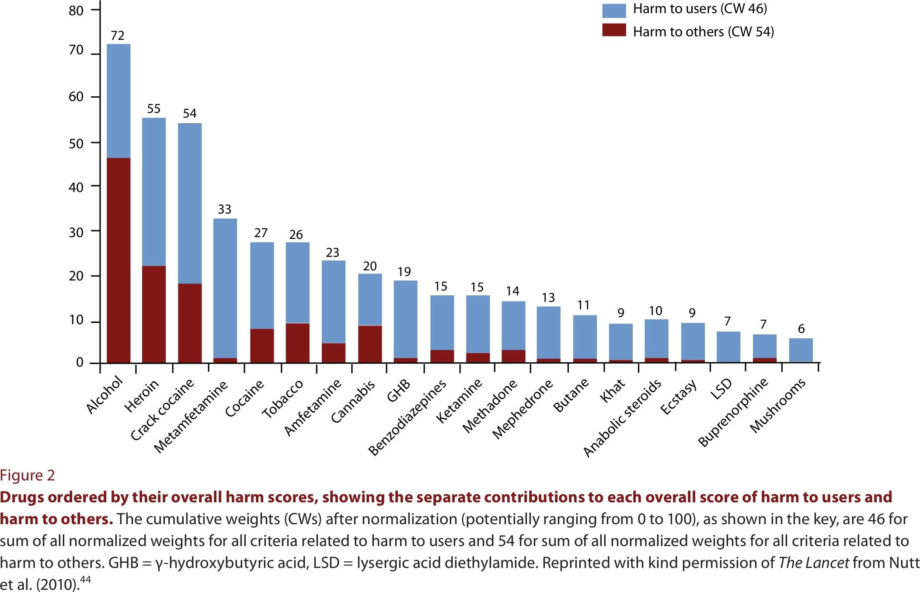
Wood E, McKinnon M, Strang R, Kendall PR. Improving community health and safety in Canada through evidence-based policies on illegal drugs. Open Medicine. 2012;6(1):e35-e40.
Regarding the harm each drug causes, heroin, crack cocaine, and methamphetamine are the most harmful drugs to individuals, whereas alcohol, heroin, and crack cocaine are the most harmful to others. Overall, alcohol is the most harmful drug with heroin and crack cocaine in second and third places.
The following chart Comparing Dangers of Popular Drugs illustrates the dangers of six different drugs based on five criteria, being:
Withdrawal: Presence and severity of characteristic withdrawal symptoms.
Reinforcement: A measure of the substance’s ability, in human and animal tests, to get users to take it again and again, and in preference to other substances.
Tolerance: How much of the substance is needed to satisfy increasing cravings for it, and the level of stable need that is eventually reached.
Dependence: How difficult it is for the user to quit, the relapse rate, the percentage of people who eventually become dependent, the rating users give their own need for the substance and the degree to which the substance will be used in the face of evidence that it causes harm.
Intoxication: Though not usually counted as a measure of addiction in itself, the level of intoxication is associated with addiction and increases the personal and social damage a substance may do.
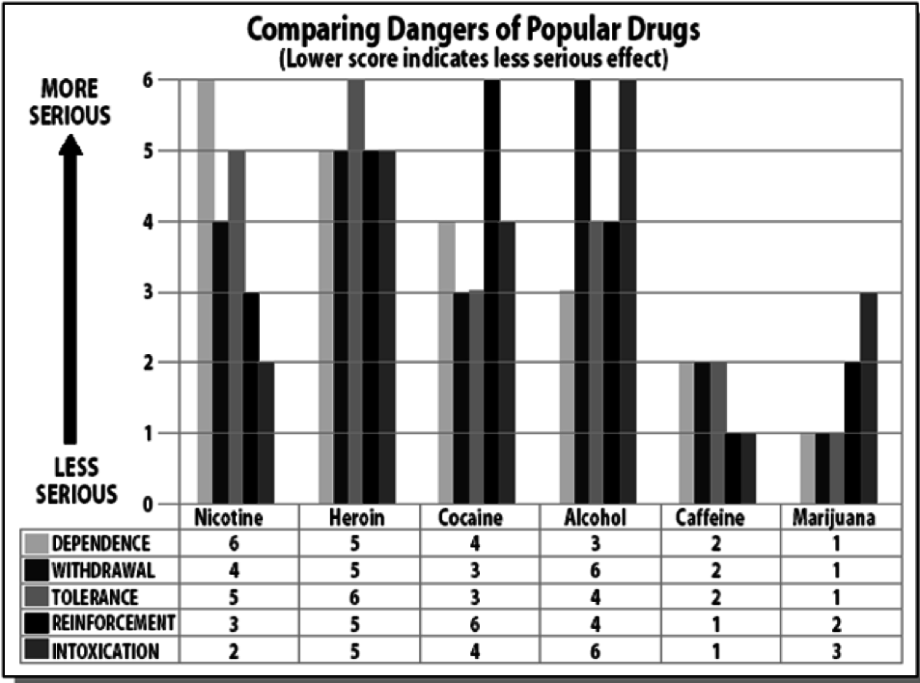
Source: Jack E. Henningfield, PhD for NIDA, Reported by Philip J. Hilts, New York Times, Aug. 2, 1994 “Is Nicotine Addictive? It Depends on Whose Criteria You Use.”
http://www.nytimes.com/1994/08/02/science/is-nicotine-addictive-it-depen…
http://www.erowid.org/psychoactives/addiction/addiction_media1.shtml
A significant percentage of the population is addicted to nicotine (14.6% from Tobacco Use in Canada: Patterns and Trends, 2015 Edition) but it rarely hijacks someone’s life. What makes nicotine the most addictive drug, but not the most impairing? Although nicotine is very addictive, it does not intoxicate or reinforce itself as much as other substances.
Route of Administration (how quickly drugs work)
The faster a drug reaches your brain, the higher the risk of addiction. The fastest way for a drug to reach your brain is if you inject it, then if you smoke, snort or swallow it, in that order. The method used to consume a drug is called the “route of administration”. Some drugs affect the brain within seconds of use. Drugs that are smoked or injected reach the brain very quickly and result in an intense but short-lasting high. These drugs are highly addictive and include methamphetamine, cocaine, crack cocaine and heroin.
Severity of Withdrawal Symptoms
Some drugs are particularly addictive because they result in severe withdrawal symptoms if stopped. Prolonged use of a drug can lead to tolerance, or a lessening of the drug’s effects due to changes in the brain. Tolerance is a sign of physical dependency on a drug, meaning that withdrawal symptoms will be experienced if the drug use is discontinued. It is important to note that physical dependency and addiction are not the same thing; addiction has a psychological component that results in a compulsion to use a drug and cravings for the drug even in the absence of withdrawal symptoms. However, drugs that result in severe withdrawal symptoms can be among the most addictive, as the unpleasant symptoms of withdrawal encourage continued use (reinforce consumption).
For drugs that quickly leave the bloodstream, like cocaine, withdrawal symptoms can appear within hours. These symptoms often include depression, anxiety, and a craving for the drug. If these feelings are strong enough, they can drive a person to continue using the drug despite significant adverse consequences—the definition of addiction.
There are a number of factors that determine the addictive potential of drugs. Some of the most addictive drugs are the nicotine in tobacco, heroin, crack cocaine, cocaine, alcohol, methamphetamine, crystal meth – all of which are either smoked, injected intravenously, have severe withdrawal symptoms, and/or result in a quickly-developed tolerance.